Shock Index Calculator
The Shock Index is a quick bedside tool used to assess a patient’s hemodynamic stability. It is calculated by dividing the heart rate by the systolic blood pressure. A higher value may indicate early shock, helping clinicians identify patients at risk of poor outcomes.
Shock Index Calculator is intended for informational and educational purposes only. It should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider.
What is Shock?
Shock is know as a serious medical condition that occurs when the human body does not get the right amount of blood flow. This conditions causes to the important organs that include brain and heart to have insufficient amount of oxygen and nutrients. In conditions like this of the medical treatment isn’t done on time it might result in organ failure or death. Some of the most typical symptoms that might occur are fast or weak pulse, shallow breathing, clammy or chilly skin, disorientation, and low blood pressure.
Different conditions or causes that shock can result include heavy bleeding, heart issues, serious infections, allergic responses, damaged nerves, and restricted blood flow. This type of medical condition is an emergent one that needs a call for emergency services, keeping the patient warm and raising their legs until the medical assistance comes. This is a medical emergency that needs to be treated right away.
What is Shock Index?
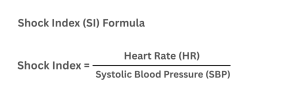
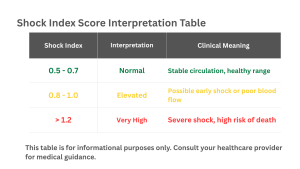
Shock index is an simple bedside calculation for identifying early shock symptoms. It can be calculate in very simple way by dividing the systolic blood pressure (SBP) by the heart rate (HR), below you will have the shock index formula. If form the calculation the score may be above 1.0 it indicates poor blood circulation and an increased risk of major problems or mortality, but for values that are from 0.5 to 0.7 is considered a normal range.
The shock.index assists healthcare providers in determining which patients require immediate medical care, especially in cases of trauma, sepsis, heart attacks, or severe bleeding. It is an easy and quick tool that doesn’t require any extra special tool that is done fast only by accessing vital sings. Due to its accuracy and speed is commonly used for advising early medical treatment decisions in critical care and emergency centers.
Clinical Use of Shock index?
Considered as quick rapid bedside method in clinical use the shock index is used to detect early or hidden shock, in particular form trauma and hemorrhage situations. Increased shock index values assits in determining the requirement for large transfusions, vasopressor support, and increased mortality risk. It helps in tracking how well the fluid resuscitation is working, persistent rise indicates instability. In cases where some vital sings may seem normal in sepsis, shock.index may be used as an extra indicator if tissue perfusion. It is useful in emergency and prehospital triage situations due to its ease of use and fast calculation.
Advantages of Shock index
Shock index is a method for detecting the early indicators for circulatory failure before blood pressure drops. Its assistance in detecting and giving the chance for quicker responses and better patients outcomes for compensated shock is a big advantage and help. Due to the combination of systolic blood pressure and heart rate it gives a more sensitive evaluation than just looking separately on vital sings.
In cases of trauma and sepsis, it also estimates the need for transfusions, surgery, or intensive care unit care. The shock.index is easy to use, affordable, and perfect for quick triage, particularly in situations with limited resources or emergency. A patients progress can be tracked with repeated measures, and newer and modified versions such as MSI, ASI, and SIPA are helpful for wide range of age groups and medical problems.
Limitations of Shock Index
Beside being a simple and helpful tool, it comes along with some limitations. It has a limit for specificity in determining precise type of shock, and also can be affected from conditions such as drugs, fever, or physical training, which change blood pressure and heart rate. The accuracy of shock index can vary for different patients groups like elderly or those with chronic illnesses, and it does not directly assess tissue perfusion or oxygen supply. Not enough research has been done to determine how effectively SI functions in real-world situations, and there isn’t a single, definitive value that identifies an unusual SI.
Interpretation in Special Scenarios
Children: The typical SI values for adults don’t apply to children since they have lower blood pressure and quicker heartbeats.
Sepsis: SI can be deceptive in infections because extended blood arteries, not blood loss, cause low blood pressure.
Neurogenic shock: Even in cases of severe shock, a slow pulse and low blood pressure can make SI appear normal.
FAQS for Shock Index
Can the Shock Index predict mortality or other adverse outcomes?
Yes. A high Shock Index (SI) often means a patient is at greater risk of serious problems, like death, needing a blood transfusion, or a longer ICU stay. In trauma, a higher SI usually signals the need for urgent interventions and more hospital resources.
How does the Shock Index perform compared to standard vital signs alone?
The SI is often better at spotting early shock than just looking at heart rate or blood pressure by themselves. Sometimes a patient’s blood pressure looks normal while their heart rate is high—SI can catch this imbalance and give an early warning.
What is the role of the Shock Index in prehospital or EMS settings?
EMS teams can use the SI to quickly figure out which patients are unstable and need urgent care. A high SI before reaching the hospital can alert staff to prepare for treatments like transfusions or surgery.
How do medications like beta-blockers affect the Shock Index?
Beta-blockers lower heart rate, so the SI may appear normal even if the patient is in trouble. Doctors need to interpret SI carefully, considering medications and overall patient condition.
Can the Shock Index be used for conditions other than trauma?
Yes, the Shock Index is also useful in sepsis, heart attacks, pulmonary embolism, and obstetric emergencies. A high SI can indicate rapid blood loss or worsening organ function. It helps clinicians identify patients at risk and act early.
How does the Modified Shock Index (MSI) differ from the standard Shock Index (SI)?
The MSI uses heart rate divided by mean arterial pressure instead of systolic blood pressure. Some studies suggest it may better predict outcomes in conditions like sepsis. It’s a useful alternative when a more accurate risk assessment is needed.
How can repeated Shock Index measurements be used?
Watching SI over time shows trends. If it stays high or rises, the patient may be getting worse. If it drops, the patient is likely responding to treatment.
Is there an age-adjusted Shock Index for older adults?
Yes. Older adults may not show typical signs of shock, so some studies adjust SI for age. Doctors should interpret SI carefully in elderly patients.
Can the Shock Index be used to guide treatment decisions, like fluid resuscitation?
Yes. A high SI can indicate the need for fluids, transfusions, or medications like vasopressors. But it should always be considered along with other clinical information, not used alone.
What is the evidence supporting the use of the Shock Index?
Many studies support using SI in trauma, sepsis, and other conditions. It often predicts problems earlier than single vital signs. However, large prospective studies are limited, so SI is best used as an additional tool rather than the sole guide.
Explore More Helpful Health Tools
We develop tools to help you take control of your well-being and make informed life choices. Explore our range of health resources, including our Shock Index Calculator, designed to support your mental and physical health.
Below you will find a couple of them and much more that are just a search away . If you don’t find any specific test or calculator you’re looking for please feel free to contact-us so we can create it for everyone.
Revised Trauma Score (RTS)
A scoring system that uses vital signs and consciousness level to assess trauma severity and predict patient outcomes.
COPD Assessment Test (CAT)
A simple questionnaire that evaluates the impact of COPD on a patient’s daily life and symptoms.