BISAP Score for Pancreatitis Mortality
The BISAP (Bedside Index for Severity in Acute Pancreatitis) score is a quick and easy tool doctors use to assess how severe a case of acute pancreatitis might become. By checking five simple factors within the first day of hospital admission, it helps identify patients who are at higher risk of complications or death. This allows healthcare providers to act early and give the right level of care when it’s needed most.
The calculator is intended for informational and educational purposes only. It should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider.
Understanding Acute Pancreatitis
Acute pancreatitis is an unexpected inflammation of the pancreas than can vary from a minor, self-limiting illness to a serious life threating condition. Since immediate action can greatly improve the outcome, its important to evaluate patients at risk for serious complications or mortality as soon as possible. Some different evaluation scoring methods such as the BISAP Score and Ranson Criteria, have been created to help healthcare providers to evaluate the high risk patients (cases). These systems offer objective measurements to direct patient care.
What is the BISAP Score?
BISAP Score (Bedside Index for Severity in Acute Pancreatitis) is a fast and accurate bedside method for determining the severity of acute pancreatitis within the first 24 hours of hospital admission. It allows for early intervention and improves care by helping doctors in identifying patients who are more likely to have problems, organ failure, and mortality. BISAP score provides a high prediction accuracy for patients results, and compared to other methods is simple to understand, cost-effective and useful. Because of its simplicity of use, it can be especially useful in busy clinical situations where quick decisions are essential.
History and Development of the BISAP Score?
The BISAP Score was created in the early 2000s in order to evaluate the patients with acute pancreatitis who where at high risk of mortality in the hospital. It was developed using a dataset of over 18,000 cases that were gathered from more than 200 hospitals between 2000 and 2001. Also, from this data set was noticed that 5 predictive factors where nedded to evaluate within the first 24 hours. Later, form 2004 to 2005 about 18,000 more cases from 177 different hospitals were used to validate the score, demonstrating its accuracy. BISAP Score for pancreatitis was created as an simple bedside method that offered a simpler option compared to other more complex evaluation methods without sacrificing predictive accuracy.
Components of the BISAP Score
- B: BUN >25 mg/dL
- I: Impaired mental status (Glasgow Coma Scale <15)
- S: SIRS (Systemic Inflammatory Response Syndrome) ≥2
- A: Age >60 years
- P: Pleural effusion on imaging
Clinical Use of BISAP Score?
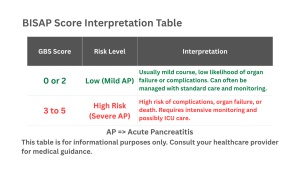
BISAP Score is used within the first 24 hours of receiving medical care, to quickly evaluate patients that are at risk for severe acute pancreatitis and mortality. It allows for effective recourse allocation, predicts the results for high score that are related with a worse prognosis, and assists in guiding medical treatment decisions such as ICU admission or increased monitoring. The simplicity of it as a practical bedside tool make it a useful method when compared with other complex scoring systems. It helps healthcare providers to tale early actions and avoid difficulties in their daily practice. By offering a precise, uniform indicator of severity, the score enhances communication across medical teams.
Advantages of BISAP Score?
BISAP Score for pancreatitis offers several benefits of using it while treating patients with acute pancreatitis. The simplicity and being easy to use helps healthcare providers to quickly estimate it at the patients bedside using easily accessible clinical and laboratory data within the 24 hours of admission. Total score allows for early medical treatment and for better patients results by determining an accurate mortality rate, organ failure and severe illnesses. While it saves time and recourses, it is cost-effective, and has predictive accuracy that is comparable to more complex methods such as Ranson’s Score. It can be quickly used at the bedside to identify high-risk patients who need closer monitoring or care in the ICU.
Limitations of BISAP Score?
The score comes along with some limitations that include limited sensitivity and d inconsistent accuracy in predicting acute pancreatitis or organ failure that may miss severe cases. It may perform differently in different populations groups and researches, and it can occasionally fall outside of the best window for early intervention. There is a chance of false negatives that might postpone necessary medical treatment, and additional validation is required to guarantee consistent dependability in clinical practice. Also, it is less successful in identifying every patient who would need advanced care or close monitoring.
FAQs for BISAP Score
Can the BISAP score be used for children?
No. The score was created using data from adults and hasn’t been validated for children. For pediatric cases, the Pediatric Acute Pancreatitis Severity (PAPS) score is a more suitable tool, as it’s designed specifically for younger patients.
Does the BISAP score give a definite diagnosis of severity?
No. The score is meant for early risk assessment, not a final diagnosis. It helps estimate the likelihood of severe disease but should always be used alongside imaging, lab results, and the patient’s overall clinical evaluation. .
What does the “B” in BISAP stand for? Why does it matter?
The “B” represents Blood Urea Nitrogen (BUN) > 25 mg/dL. High BUN levels indicate dehydration, systemic inflammation, or kidney issues , all of which are linked to more severe outcomes in acute pancreatitis. .
How does mental status affect the BISAP score?
Impaired mental status (Glasgow Coma Scale score below 15) is one of the five BISAP criteria. It can signal early organ dysfunction or systemic illness. A patient with reduced mental alertness earns one point on the BISAP score, reflecting a higher mortality risk. .
How is the BISAP score used in the Emergency Department (ED)?
The score is highly useful in the ED because it can be calculated quickly with information available in the first 24 hours. It helps identify patients at higher risk who may need intensive monitoring, rapid treatment, or transfer to a specialized center. .
Is the BISAP score more accurate than imaging in predicting severity?
Not exactly. Imaging, like CT scans, helps detect local complications such as pancreatic necrosis but usually happens later. The score complements imaging by offering an early, systemic risk prediction using basic clinical data. .
Do other factors influence BISAP’s accuracy?
Yes. While the score focuses on five main criteria, other aspects, such as the cause of pancreatitis (alcohol, gallstones) or existing conditions like diabetes and heart disease, can also affect patient outcomes. BISAP is a helpful guide but should always be interpreted in the full clinical context. .
Explore More Helpful Health Tools
Our website is here to create tools that help people to make better life choices and having your body and mind in control. We provide a range of health related tools like the BISAP Score Pancreatitis tool designed to support your well-being.
Below you will find a couple of them and much more that are just a search away . If you don’t find any specific test or calculator you’re looking for please feel free to contact-us so we can create it for everyone.
Glasgow Coma Scale (GCS Score)
A tool used to assess a patient’s level of consciousness based on eye, verbal, and motor responses.
Ranson’s Criteria for Pancreatitis Mortality
A clinical scoring system used to predict the severity and risk of death in acute pancreatitis.