Glasgow-Blatchford Bleeding Score (GBS)
The Glasgow-Blatchford Score (GBS) is a tool doctors use to see how serious an upper gastrointestinal bleed is. It looks at things like vital signs, blood tests, and medical history to quickly tell who can be safely treated as an outpatient and who needs to stay in the hospital. This helps doctors decide on the right care and act fast in emergencies.
GBS Score Calculator is intended for informational and educational purposes only. It should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider.
What is Upper Gastrointestinal Bleeding (UGIB)?
Upper Gastrointestinal Bleeding (UGIB) is a serious medical emergency that may come from different causes like bleeding from the duodenum, stomach, or esophagus. Some of the present symptoms that a patient may come is vomiting with blood(hematemesis), melana (black or tarry feces), hematochezia (recotal bleeding), dizziness, or fainting from blood loss. Also, among the common causes may be liver diseases that are related to variceal bleeding, esophagitis, duodenal or stomach erosions, vascular ectasias, Mallory-Weiss tears and tumors.
When a patient is being diagnosed it typically they need to have medical records, physical examination, blood tests, and endoscopy to determine the cause of the bleeding. The medical treatment of patients aims to prevent bleeding and maintain the patient into a stable state. The process can include to give fluidsthrough a vein (IV),using medication to lower stomach acid, and in more severe situations having surgery or specialized imaging tests.
Challenges in Emergency Management of UGIB
In an emergency room, controlling upper gastrointestinal bleeding might be challenging. Some of the most concerning situations may be stabilizing patients in shock with fluids or blood transfusions, prrotecting the respiratory system in patients who are vomiting or have reduced awareness to avoid aspiration. To have a good start in having the proper diagnose and medical treatment is an early endoscopy, but it should only be performed after suitable resuscitation. Risk scoring evaluation methods have their impact on determining which patients are low-risk and which require immediate medical care.
Patients who are taking blood thinners or antiplatelets or who have other medical conditions require special attention because stopping and continuing these medications can be dangerous. The bleeding is normally stopped by endoscopic treatments, but occasionally the bleeding might start again. In the cases where the endoscopy fails, the patients may need through a surgery, which is more dangerous. Some cases that may be very serious can be required treatment in intensive care unit (ICU), and in place with lower medical facilities, access to advanced care and endoscopy may be limited, which can result in increased mortality..
Role of Risk Scoring Systems for UGIB
Risk scoring methods used for upper GI bleeding give an assists to doctors in making fast decisions about the patients depending in what state they can be. The state they may is in high risk and they require immediate endoscopy and hospital treatment, and those in low risk and suitable for outpatient care. Important outcomes such as the requirement for a blood transfusion, the possibility of bleeding again, hospitalization, and mortality are predicted by these scores.
Some of the methods are the Glasgow-Blatchford Score (GBS), which assists in determining which patients are safe for outpatient treatment and which require intervention, The Rockall Score, which calculates the probability of bleeding again and mortality rate, and the AIMS65 Score which predicts in-hospital mortality. Beside being very helpful, none of these methods are perfect,which means patient outcomes may vary. To improve the accuracy of risk prediction, newer techniques like machine learning and artificial intelligence are being studied.
What is Glasgow-Blatchford Bleeding Score (GBS)?
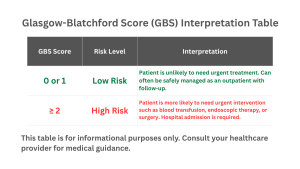
Glasgow Blatchford Score (GBS) is a medical method used to determine the degree of upper gastrointestinal (GI) bleeding before doing the endoscopy. GCS score is based on basic clinical data, including vital signs, symptoms, medical history, and blood test result. A high score from Blatchford score indicates that hospital treatment is needed endoscopy, or other procedures, but for low scores (especially 0) indicates that patients can be handled properly as an outpatients. Its primary advatnage is its fast calculation, which eliminates the need for endoscopy and makes it highly useful in emergency situations. Patient safety is increased and unnecessary hospital stays are lower by the glasgow blatchford score, which provides guidance for early admission and treatment decisions.
History and Development of the Glasgow Blatchford Score (GBS)
The Glasgow Blatchford Score (GBS) was first introduced by its creator Oliver Blatchford and his calleagues in 1997,Glasgow as a method for evaluating the patients suffering from UGIB. Its creation was designed to reduce unnecessary hospitalizations by identifying low-risk patients who might be safely treated as outpatients. GBS score firstly was based on large studies in patients, it included simple clinical and laboratory data to evaluate early decision-making. The GBS score gained international recognition over the years, was included into medical recommendations, and was revised into other versions such as the modified GBS (mGBS), which also improved its use in emergency treatment.
Components of Glasgow Blatchford Score
Clinical Factors:
- Presentation with melena
- Presentation with syncope
- Systolic blood pressure
- Heart rate
- Comorbidities: liver disease, cardiac failure
Laboratory Factors:
- Hemoglobin (based on gender)
- Blood urea / BUN
Clinical use of GBS Score
In emergency situations, the Glasgow Blatchford Score is mostly used for evaluating the patients who may have UGIB and inform for medical treatment options. As me mentioned before that for high risk scores it indicated the possibility for hospitalizations and procedures like endoscopy or blood transfusion, and for low risk ones that they can be treated as outpatients. Blood tests, vital signs, and patient history are examples of basic non-endoscopic procedures that the GBS score uses to cut down on unnecessary admissions, enhance triage, and guarantee prompt treatment for patients who are more vulnerable.
Advantages of Glasgow Blatchford Score
Glasgow-Blatchford Score have some advantages used to treat upper gastrointestinal bleeding (UGIB). The low score patients who may be safely treated as outpatients by offering an early, objective assessment without the need for endoscopy is one of the benefits. This helps in ensuring and preventing unnecessary hospital stays, lower medical treatment costs, and guarantees that resources are directed to high-risk patients. The GBS Score helps in making decisions and improving the outcomes by identifying the need for medical treatment for patients like endoscopy or transfusion. As an easy to use method and that it depends on standard clinical data also makes it simple to include into common emergency treatment.
Limitations of GBS
The Glasgow-Blatchford Score (GBS is a useful method for evaluating upper gastrointestinal bleeding (UGIB), but it comes along with some limitations. The score may underestimate the patients risk since it ignores some risk factors and comorbidities, like chronic liver disease, alcohol withdrawal, or respiratory issues. Compared to other scoring methods or tools, the score is less reliable for variceal hemorrhage and has a limited capacity for predicting death. The dependence on subjective factors and incomplete clinical data decreases its consistency and utility across various patient groups. Because of some the limitations we mentioned, doctors usually combine the score with other methods or tools such as Rockall or AIMS65.
FAQs for the Glasgow-Blatchford Score (GBS)
Can the GBS be used if a patient is actively bleeding?
Yes. The score can be calculated even during active bleeding since it relies on vital signs and blood tests. A higher score usually means the bleeding is more severe and urgent care is needed.
Is the score calculated differently for men and women?
Yes. Hemoglobin scoring is adjusted for sex, since normal levels differ between men and women.
Why does the score include blood urea nitrogen (BUN)?
When there’s a major upper GI bleed, blood proteins get broken down and absorbed, which raises urea levels. High BUN often signals a heavier bleed.
Does the GBS predict mortality?
Not directly. The GBS mainly predicts who needs treatment like transfusion or endoscopy. Higher scores may link to higher risk of death, but tools like the Rockall or AIMS65 score are better for predicting mortality.
Has the GBS been tested in different countries?
Yes. It has been widely studied around the world and is recommended by international guidelines, especially in the UK and Europe. It works well in many hospital settings, including ERs.
If someone has a GBS of 0, can they still have a serious problem?
Yes. A score of 0 means they are very unlikely to need urgent treatment, but it doesn’t rule out issues like gastritis, esophagitis, or even varices or cancer. Follow-up is still important.
Does the GBS predict rebleeding?
Not very well. It’s best at predicting the need for the first intervention. For rebleeding risk, other scoring tools and clinical judgment are more reliable.
More Tools to Support Your Health
Our website is dedicated to providing tools that empower you to make informed health choices and take control of your body and mind. We offer a variety of health-related calculators, including the GBS Score Calculator, to support your overall well-being.
Explore the tools below and many more, just a search away. If you don’t find a specific test or calculator, feel free to contact us, and we’ll be happy to create it for everyone.
Glasgow Coma Scale (GCS)
Assesses a patient’s level of consciousness after a head injury.
Revised Trauma Score (RTS):
Evaluates trauma severity to predict patient survival and guide emergency care.